38 year old male with chief complaints of pain abdomen
A 38 year old male came to the casuality with chief complaints of pain abdomen since 15 days and nausea w vomitings since 3 days (8-10 times/day) it was bilious and associated with blood
HOPI
Pt was apparently asymptomatic 3 years back when he developed abdominal pain - squeezing type, aggravated with food intake with no relieving factors and no radiations.
For which he was previously admitted in the hospital, stayed for a week and was discharged.
H/o similar complaints in past on and off relieved only on pain medication once in 2-3 months.
Currently he presented with left sided flank pain dragging type, radiating to the back, relieved on lying in left lateral position, aggravated with food intake. Associated with nausea, vomiting, associated with food particles, non bilious, not associated with blood.
PAST HISTORY
No H/o HTN, DM, TB, Asthma, Epilepsy, CVA, CAD, thyroid disorders
PERSONAL HISTORY
Pt is a known Alcoholic with history of drinking since 15 years (180-360ml) daily. Appetite - Highly reduced Diet - Mixed. Bowel and Bladder - Regular and normal. Sleep - Disturbed. Other addictions - Chewable tobbaco 1 pack for evey two days since 10 years.
FAMILY HISTORY
Not applicable
ON EXAMINATION
Patient was conscious/coherent/cooperative
Pt looks severely malnourished
Pallor, Icterus, Cyanosis, Clubbing, Lymphadenopathy, Oedema of feet are all absent
Temperature - 97.6. Pulse Rate - 82 BPM. Respiratory rate - 24 cpm. Blood pressure - 110/70 mm Hg.
CNS EXAMINATION
HMF normal
CVS EXAMINATION
S1 S2 heard, no murmurs heard.
RS EXAMINATION
Normal respiratory sounds heard
PER ABDOMEN
Scaphoid shaped abdomen with tenderness in left flank which is radiating to left back.
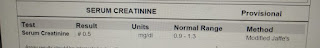
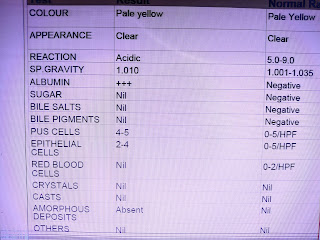
INVESTIGATIONS
19/07


TREATMENT
Day 1
1) IVF- 3 NS and 2 RL @ 125ml/hr
2) INJ Pan 40mg IV/OD
3) INJ Tramadol in 100ml NS IV/SOS
4) INJ Zofer 4mg IV/TID
5) TAB Creon 10,000 IU PO/TID 30 min before food
6) INJ Thiamine in 100ml NS/IV/BD
7) NBM till further orders
Day 2
1) IVF- 3 NS and 2 RL @ 125ml/hr
2) INJ Pan 40mg IV/OD
3) INJ Tramadol in 100ml NS IV/SOS
4) INJ Zofer 4mg IV/TID
5) TAB Creon 10,000 IU PO/TID 30 min before food
6) INJ Thiamine in 100ml NS/IV/BD
7) TAB Lorazepam 2 mg (one tablet in the morning two at night)
8) Nicotex gums
9) NBM till further orders
Day 3
1) IVF- 3 NS and 2 RL @ 75ml/hr
2) INJ Pan 40mg IV/OD
3) INJ Tramadol in 100ml NS IV/SOS
4) INJ Zofer 4mg IV/TID
5) TAB Creon 10,000 IU PO/TID 30 min before food
6) INJ Thiamine in 100ml NS/IV/BD
7) TAB Lorazepam 2 mg (one tablet in the morning two at night)
8) Nicotex gums
9) Allowing liquid diet
Day 4
1) IVF- 3 NS and 2 RL @ 75ml/hr
2) INJ Pan 40mg IV/OD
3) INJ Tramadol in 100ml NS IV/SOS
4) INJ Zofer 4mg IV/TID
5) TAB Creon 10,000 IU PO/TID 30 min before food
6) INJ Thiamine in 100ml NS/IV/BD
7) TAB Lorazepam 2 mg 2 tablets at night
8) Nicotex gums
9) Allowing soft diet
10) INJ Monocef 1g IV/BD















Comments
Post a Comment