Medicine case discussion
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent
Here we discuss our patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs
This E log book also reflects my patient - centered online learning portfolio and your valuable inputs inthe comment box are welcome
I have been given this case to solve an attempt to understand the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
CHIEF COMPLAINTS
A 38 year old female came to the OPD with chief complaints of Shortness of breath and B/L swelling of limbs
HISTORY OF PRESENTING ILLNESS
Pt was apparently asymptomatic 3 months back when she shortness of breath, gross ascites and pedal edema
She is a K/C/O CKD on MHD since 3 months
K/C/O HTN since 3 months
Pt presented for the first time 3 months back with complaints of decreased appetite, bilateral swelling of lower limbs, she was already a k/c/o CKD on MHD. Asymptomatic till 1 month before she developed decreased appetite along with b/l swelling of lower limbs, no c/o SOB back then and she wasn't Hypertensive as well.
Pt presented for the second time 2 months back with complaints of SOB, B/L pedal edema and was hypertensive.
Pt presented for the third time one month back with complaints of SOB, Gross ascites and pedal edema.
Pt presented three days back with chief complaints of SOB and b/l pedal edema
PAST HISTORY
No history of DM, TB, Asthma, Epilepsy, CVA, CAD.
Pt was not hypertensive three months back but developed HTN three months back.
PERSONAL HISTORY
Appetite - reduced
Diet - mixed
Bowel and bladder - normal
Built - malnourished
Sleep - regular
Addictions - no known addictions
FAMILY HISTORY
Pt own mother reportedly had similar complaints and was also a CKD patient. Might indicate familial tendency of kidney disease.
ON EXAMINATION
Pt is Conscious, Coherent and Co operative
Pallor - present
Icterus - present
Cyanosis - absent
Clubbing - absent
Koilonychia - absent
Pedal edema - bilaterally present
Pt is severely malnourished showing mild dehydration
Temp - Afebrile
PR - 82 BPM
BP - 140/100 mm Hg
RR - 21 cpm
CNS Examination
No Focal deficit seen
HMF normal
CVS Examination
S1 and S2 heard
No murmurs
RS Examination
Normal vesicular breath sounds
Per Abdominal examination
Slightly distended abdomen
INVESTIGATIONS
13th July
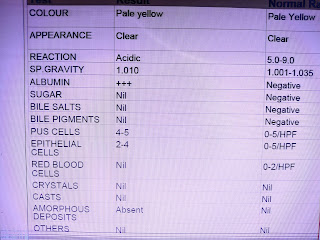
Complete Urine Examination
Blood Urea
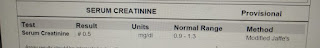
Serum Creatinine
Serum Iron
Complete Blood Picture
ABG
14th July
Hemogram
Renal Function Test








Comments
Post a Comment